News
-
![]()
3D-printed superconductor achieves record performance
Nearly a decade after they first demonstrated that soft materials could guide the formation of superconductors, Cornell researchers have achieved a one-step, 3D printing method that produces superconductors with record properties.
-
![]()
Biodegradable ‘heat bombs’ safely target specific cells
Cornell researchers developed a new way to safely heat up specific areas inside the body by using biodegradable polymers that contain tiny water pockets, a technology that could lead to precise and noninvasive diagnostics and therapeutics.
-
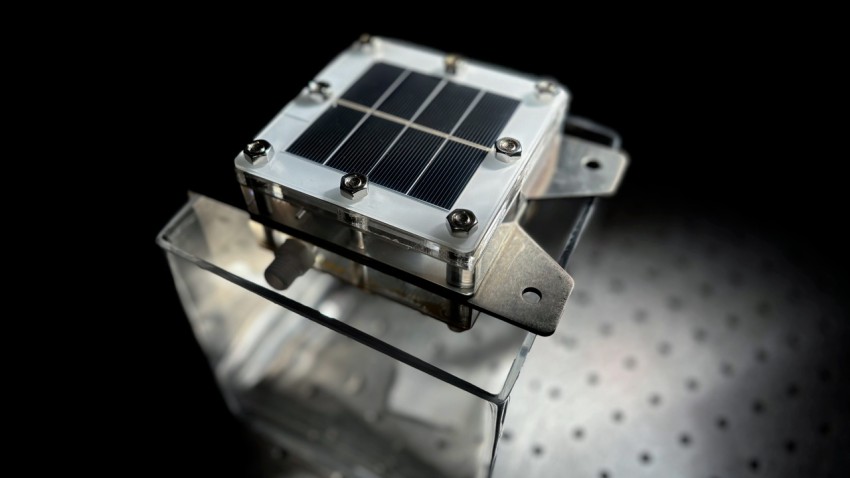
![A Cornell-led team built a 10 centimeter by 10 centimeter prototype device that produces carbon-free “green” hydrogen via solar-powered electrolysis of seawater, with an important byproduct: potable water.]()
Sunlight and seawater lead to low-cost green hydrogen, clean water
Researchers developed a low-cost method to produce carbon-free “green” hydrogen via solar-powered electrolysis of seawater, with a helpful byproduct: potable water.
Latest Awards and Recognition
View all-
Three research teams receive grants
Three Cornell engineering research teams have been chosen as recipients of AI and Climate Fast…
December 1, 2025
-
Barcheck, Culberg earn NSF award for field study
Grace Barcheck, assistant professor, and Riley Culberg, assistant professor, have received an award from the…
November 25, 2025
-
Trio named Engaged Faculty Fellows
Three Cornell Engineering faculty members are part of the 2025-26 Engaged Faculty Fellows cohort.
November 24, 2025
-
You paper featured on Chemical Science cover
Fengqi You, the Roxanne E. and Michael J. Zak Professor in Energy Systems Engineering, had…
November 17, 2025